Reasons not to believe in lithium
Lowe took lithium from the age of 17 for 20 years, until at the age of 37 or thereabouts she was diagnosed with kidney failure, a direct result of this treatment. She will need dialysis, and a kidney transplant – a high price to pay for a really effective treatment. The sad thing is, we have little evidence that lithium is a really effective treatment, or even that it is effective at all. However, as I explain below, once someone starts on lihium, there is evidence that there is a high risk of having a relapse if they stop it. This is not the same as showing that lithium is a good thing in the first place, but it does mean that people who are already taking lithium have to be very careful if they decide they want to come off.
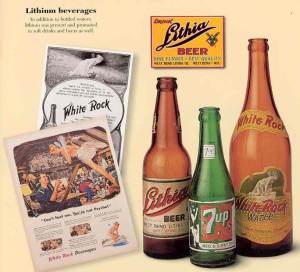
Lithium is a neurotoxin. It inhibits the functioning of the nervous system so that people typically feel drowsy, lethargic and slowed up. These effects were observed in guinea pigs initially, and then in people with mania by the Australian doctor, John Cade, who first proposed that lithium might be a useful treatment for manic depression (1). In the 19th century lithium had been used for the treatment of gout, and became a popular ingredient of tonics and even beer, until it was shown that it did not dissolve the uric acid crystals that cause gout as had been claimed (2).
The sedative and slowing effects of lithium, although usually described as side effects, account for why lithium can help reduce arousal and activity levels in people with acute manic symptoms. So there is nothing magic or specific about lithium’s action in manic depression. Lithium will exert its characteristic effects in anyone, whether or not they have mania or manic depression. In theory, these effects might suppress the emergence of a manic episode, as well as reduce the severity of symptoms once an episode has started. The evidence that long-term lithium treatment reduces the occurrence of manic or depressive episodes is actually very weak, however.
The main problem with the evidence is that there is no study in which people who have been started on lithium have been compared with people who haven’t. Every randomised trial of lithium versus placebo starts with people who are already on drug treatment of one sort or another, often lithium itself. Now there is good evidence, accepted by leading proponents of lithium (3;4), that withdrawing from lithium can precipitate a relapse of manic depression, especially a manic episode. Three studies have shown, for example, that people are more likely to have a relapse after stopping lithium than they were before they started it (5-7). No one knows the mechanism for this, but it is as if removing the neurological suppression produced by lithium causes the nervous system of a susceptible person to go into over-drive, precipitating a manic relapse.
So demonstrating that people who stop lithium and start a placebo have higher rates of relapse than people who continue on lithium does not demonstrate that going onto lithium in the first place prevents episodes. But all the placebo-controlled trials of lithium are like this to at least some degree. The trial that established the idea of long-term lithium treatment, for example, started with people who had already been on lithium for many years (8). In more recent studies, not all participants have been on lithium prior to enrolment, but those not taking lithium were likely to be taking other sorts of sedative medication. The first of these recent studies, the largest study up until that point involving 372 participants, found no difference between lithium, sodium valproate and placebo in terms of the rate of recurrence of any type of mood episode (9). The second found a higher rate of manic relapse in placebo-treated patients compared with those on lithium, but the pattern with which relapses occurred was strongly suggestive of a discontinuation effect. A large majority of relapses occurred in the first few weeks after allocation to placebo, and none occurred in the last few months of the study, suggesting that the point of discontinuation of previous medication was associated with subsequent relapses (10). In the final trial, rates of mania were higher in people on placebo by about 14% (14% vs 28%), but 20% of participants were taking lithium before randomisation, and still others were taking Depakote or antipsychotics, all of which were stopped relatively abruptly prior to the trial (11).
The possibility that relapses in the placebo groups in these trials are induced by withdrawal of previous medication would make sense of the fact that it has proved impossible to demonstrate that people receiving modern drug treatment for manic depression do any better than those who don’t, or didn’t. In fact, overall, they seem to do slightly worse.
Two important studies have examined rates of relapse in people with classical manic depressive symptoms prior to the 1950s. American psychiatrist George Winokur found the records of 100 patients admitted to a psychiatric hospital between 1934 and 1944 with an episode of mania and then followed them up through their hospital records. He found that 48% had a relapse requiring hospitalisation over an average follow-up duration of 3.2 years. For comparison purposes this equates to a relapse rate of 15% per year (12). Margaret Harris, David Healy and colleagues did the same for patients admitted to the North Wales asylum in the 1890s. They found that, on average, patients had 4 relapses over the subsequent 10 years, equating to a relapse rate of 20% a year. In comparison, during the 1990s, people with manic depression (most of whom we can assume were on drug treatment) were having an average of 6.3 admissions in 10 years, or 31% per year, for example (13). That’s over 10% higher than the rate of admission for people in the 1890s!
Relapse rates among patients taking lithium in randomised trials that have started with patients experiencing a manic episode (as the historical studies did) are uniformly higher too. In the comparison between lithium, Divalproex (Depakote) and placebo, for example, the lithium group relapsed at a rate of 31% a year (9). In the comparison between lithium, lamotrigine and placebo in people with mania it was 26% a year (10). Admittedly these figures include all relapses, and not just those severe enough to require hospitalisation. A large study conducted in the 1970s, however, found that rates of hospital admission for relapse were 21.5% per year in the lithium group (14).
Several ‘naturalistic’ studies have tracked the progress of people taking lithium and other treatments. The vast majority of these studies also show high relapse rates among those on lithium, even though most studies highly compliant populations and we know that people who are compliant with any treatment (including placebo) have better outcomes than those who are not. One study of patients who were known to be compliant with their lithium treatment for at least a year, for example, found a rate of relapse of 40% a year over a 6 year follow-up (15).
In my view the evidence that lithium helps prevent episodes of manic depression is far too weak to outweigh the harms it can cause (which commonly include thyroid damage, kidney damage, and acute neurological toxicity at doses very close to those used in practice, hence the need for blood monitoring). Manic depression is a highly variable condition. Some people have many episodes, some people few, and the pattern of episodes varies throughout life as well. Long periods of remaining well are not necessarily evidence of a treatment’s effectiveness. What we would need to demonstrate the efficacy and value of lithium is a prospective randomised trial in which people who had not previously been on long-term drug treatment were randomly allocated to start lithium or placebo. At present, my view is that the evidence that lithium might be effective is not strong enough to justify such a trial, given the health risks associated with it.
As Jamie Lowe eloquently expresses, manic depression can be a terrifying condition, and I know that people will say therefore ‘if not lithium, then what?’. But the evidence that any long-term drug treatment is better than nothing is not strong (1). Many doctors and patients are very uncomfortable with that conclusion, and feel there just has to be something. And if people want to try some sort of drug treatment, like antipsychotics or anticonvulsants, then I feel that doctors should help them take it as safely as possible, at as low a dose as possible. But doctors should be honest about the state of the evidence and for lithium, I am not convinced there are any circumstances that justify the risks it entails.
In 1957 a pharmacologist bemoaned the fashion for treatment ‘by lithium poisoning’ (16). One day, I believe, we will wake up and realise his concern was spot on!
Reference List
(1) Moncrieff J. The Myth of the Chemical Cure: a critique of psychiatric drug treatment. Basingstoke, Hampshire, UK: Palgrave Macmillan; 2008.
(2) Johnson FN. The History of Lithium Therapy. London: Macmillan; 1984.
(3) Franks MA, Macritchie KAN, Young AH. The consequences of suddenly stopping psychotropic medication in bipolar disorder. Bipolar Disorders 2005;4(1):11-7.
(4) Goodwin GM. Recurrence of mania after lithium withdrawal. Implications for the use of lithium in the treatment of bipolar affective disorder. Br J Psychiatry 1994 Feb;164(2):149-52.
(5) Baldessarini RJ, Tondo L, Viguera AC. Discontinuing lithium maintenance treatment in bipolar disorders: risks and implications. Bipolar Disord 1999 Sep;1(1):17-24.
(6) Suppes T, Baldessarini RJ, Faedda GL, Tohen M. Risk of recurrence following discontinuation of lithium treatment in bipolar disorder. Arch Gen Psychiatry 1991 Dec;48(12):1082-8.
(7) Cundall RL, Brooks PW, Murray LG. A controlled evaluation of lithium prophylaxis in affective disorders. Psychol Med 1972 Aug;2(3):308-11.
(8) Baastrup PC, Poulsen JC, Schou M, Thomsen K, Amdisen A. Prophylactic lithium: double blind discontinuation in manic-depressive and recurrent-depressive disorders. Lancet 1970 Aug 15;2(7668):326-30.
(9) Bowden CL, Calabrese JR, McElroy SL, Gyulai L, Wassef A, Petty F, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 2000 May;57(5):481-9.
(10) Bowden CL, Calabrese JR, Sachs G, Yatham LN, Asghar SA, Hompland M, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry 2003 Apr;60(4):392-400.
(11) Calabrese JR, Bowden CL, Sachs G, Yatham LN, Behnke K, Mehtonen OP, et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry 2003 Sep;64(9):1013-24.
(12) Winokur G. The Iowa 500: heterogeneity and course in manic-depressive illness (bipolar). Compr Psychiatry 1975 Mar;16(2):125-31.
(13) Harris M, Chandran S, Chakraborty N, Healy D. The impact of mood stabilizers on bipolar disorder: the 1890s and 1990s compared. Hist Psychiatry 2005 Dec;16(pt 4 (no 64)):423-34.
(14) Prien RF, Caffey EM, Jr., Klett CJ. Prophylactic efficacy of lithium carbonate in manic-depressive illness. Report of the Veterans Administration and National Institute of Mental Health collaborative study group. Arch Gen Psychiatry 1973 Mar;28(3):337-41.
(15) Tondo L, Baldessarini RJ, Floris G. Long-term clinical effectiveness of lithium maintenance treatment in types I and II bipolar disorders. Br J Psychiatry Suppl 2001 Jun;41:s184-s190.
(16) Wikler A. The Relation of Psychiatry to Pharmacology. Baltimore: Williams & Wilkins Co; 1957.

Nenhum comentário:
Postar um comentário